Conditions
Medical Conditions We Treat ..
Joints & Bones
Frozen Shoulder (Adhesive Capsulitis)
Neck & Spine
Degenerative Disc Disease(DDD)
Herniated Discs(Bulging Discs)/Slipped Disc
Muscles
Brachial plexus injury
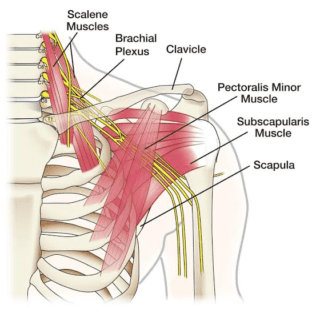
The brachial plexus is a bundle of nerves that stems from nerve roots in the cervical (neck) and upper trunk (torso) sections of the spinal cord (C5-T1), creating a network that connects to the nerves in the arm. These nerves control the motions of your wrists, hands and arms, allowing you to raise your arm, type on your keyboard or throw a baseball.
The brachial plexus nerves extend to the skin and are sensory, too. For instance, they let you know that the pan you just grabbed with your hand is too hot to hold.
The anatomy of the brachial plexus. Nerves rooted in the neck extend through the shoulders and down the arms.
The brachial plexus can be injured in many different ways — from pressure, stress or being stretched too far. The nerves may also be cut or damaged by cancer or radiation treatment. Sometimes, brachial plexus injuries happen to babies during birth.
Brachial plexus injuries cut off all or parts of the communication between the spinal cord and the arm, wrist and hand. This may mean that you can’t use your arm or hand. Often, brachial plexus injuries also result in total loss of sensation in the area.
The severity of a brachial plexus injury varies, depending on the part of the nerve that is injured and the extent of the injury. In some people, function and feeling returns to normal, while others may have lifelong disabilities because they can’t use or feel a part of their arm.
Types of Brachial Plexus Injuries
Brachial plexus injuries are categorized according to how the nerves are damaged and the severity of the injury.
Brachial Plexus Neuropraxia (Stretch)
When the nerves are stretched to the point of injury, it is referred to as neuropraxia. There are two main ways this injury occurs: compression and traction. In a compression injury, the brachial plexus nerve root is compressed, usually by the rotation of the head. Compression neuropraxia is the most common form and generally occurs in older people.
Traction neuropraxia occurs when the nerve is pulled, usually downward. This injury is less common than compression neuropraxia, but is more common among adolescents and young adults.
These types of injuries are often referred to as brachial plexus “burners” or “stingers,” depending on whether the main symptom is a burning or stinging sensation. They can also feel like an electric shock.
Brachial Plexus Rupture
In a brachial plexus rupture, a forceful stretch causes the nerve to tear, either partially or completely. This is a more serious injury than neuropraxia. Ruptures can cause weakness in the shoulder, arm or hand and can even make certain muscles unusable. These injuries can also be associated with severe pain.
Depending on the severity and location of the rupture, these injuries can often be repaired with surgery.
Brachial Plexus Neuroma
Sometimes when nerve tissue is injured, such as from a cut during surgery, scar tissue can form as the nerve attempts to repair itself. This scar tissue is called a neuroma, and it may result in a painful knot on one of the brachial plexus nerves.
Treatment for brachial plexus neuromas includes surgical removal of the scarred nerve tissue. The surgeon then either caps the nerve or attaches it to another nerve to prevent another neuroma from forming.
Brachial Neuritis
Also called Parsonage Turner syndrome, brachial neuritis is a rare, progressive disorder of the nerves of the brachial plexus. This syndrome causes sudden, severe shoulder and upper arm pain and progresses from pain to weakness, muscle loss and even loss of sensation. This syndrome usually affects the shoulder and arm, but it can also affect the legs and diaphragm. The cause of brachial neuritis is unknown, but could be related to an autoimmune response triggered by infections, injury, childbirth or other factors.
Brachial Plexus Avulsion
A brachial plexus avulsion occurs when the root of the nerve is completely separated from the spinal cord. This injury is usually caused by trauma, such as a car or motorcycle accident. More severe than ruptures, avulsions often cause severe pain. Because it is difficult and usually impossible to reattach the root to the spinal cord, avulsions can lead to permanent weakness, paralysis and loss of feeling.
Causes
Brachial Plexus Injury at Birth (Obstetric Brachial Plexus Injury)
In babies, the brachial plexus nerves in the shoulder are vulnerable during birth. Injury to the brachial plexus is fairly common during birth, occurring in one to two births per 1,000. Larger babies in difficult vaginal deliveries are particularly prone to this injury, as are babies of mothers who have diabetes.
During childbirth, large babies may be at an increased risk for brachial plexus injuries. When the baby’s head is stretched away from the shoulder, the underlying brachial plexus nerves can get injured. Babies in breech position (bottom end comes out first) and those whose labor lasts an unusually long time may also suffer brachial plexus injuries. Shoulder dystocia occurs when the shoulder is temporarily stuck under the pubis during delivery, and can result in brachial plexus injury.
Brachial plexus injury at birth generally takes one of two forms:
- Erb’s palsy: a common injury of the upper brachial plexus nerves, causing numbness and loss of motion around the shoulder and an inability to flex the elbow, lift an arm or bring objects to the mouth.
- Klumpke’s palsy: a less common injury that affects the lower brachial plexus, leading to loss of motion and/or sensation in the wrist and hand, such as being unable to move fingers.
The severity of these injuries can vary widely. Some children with brachial plexus birth injuries recover spontaneously, and most children will regain all or most of their normal function through physical and occupational therapy. A smaller group will require surgical intervention to achieve good function. Early diagnosis and treatment can improve long-term results.
Causes of Brachial Plexus Injuries in Adults
In adults, brachial plexus injuries have a range of causes, including:
- Blunt trauma:such as falls or motor vehicle accidents.
- Athletic injuries:especially from contact sports like football.
- Gunshot wounds:a bullet tears through or close to the nerves.
- Medical trauma:a nerve is cut during a surgical procedure, or damaged by an injection or the positioning of the body during surgery.
- Cancer: a tumor invades the brachial plexus.
- Radiation therapy:radiation treatment in the area damages the nerves.
Symptoms
Symptoms depend on where along the length of the brachial plexus the injuries occur and how severe they are. Injuries to nerves that root higher up on the spinal cord, in the neck, affect the shoulder. If nerves that originate lower in the brachial plexus are injured, the arm, wrist and hand are affected.
Common symptoms of brachial plexus injuries are:
- Numbness or loss of feeling in the hand or arm.
- Inability to control or move the shoulder, arm, wrist or hand.
- An arm that hangs limply.
- Burning, stinging or severe and sudden pain in the shoulder or arm.
Brachial plexus injury pain can be mild to severe, and temporary to chronic, depending on the type and extent of the injury. For instance, a simple stretched nerve may hurt for a week or so, but a ruptured nerve can cause serious, long-term pain that might require physical therapy and potentially surgery.
Diagnosis
A health care provider will examine the hand and arm and test for sensation and function to help diagnose a brachial plexus injury.
These are other diagnostic tests often used:
- An X-ray of the neck and shoulder area to identify fractures or other injuries to the bone and dense tissues around the nerves of the brachial plexus.
- Imaging tests, such as MRI or a CT scan , during which contrast dye may be injected to show the injury to the nerves of the brachial plexus.
- Tests that use needle electrodes to determine nerve function and electrical activity, including a nerve conduction study and electromyogram.
